Dorothy: [00:00:00] This woman had the world in the palm of her hand. She was looking forward to being a wife, having children, and a successful career. But that’s when she decided that having a double mastectomy and losing her breast were the best option she had for the future. What if you made this decision even when you had not developed cancer?
Well, our guest did just that. During this episode, you’ll hear why she made this difficult choice. And how the outcome was not what she expected.
Let’s Talk About Your Breast. A different kind of podcast presented to you by The Rose. The Breast Center of Excellence and a Texas treasure. You’re going to hear frank discussions about tough topics. And you’re going to learn why knowing about your breast could save your life. Join us as we hear another story and we answer those tough questions that you may have.
Our [00:01:00] guest today is someone who is a survivor, but not a survivor. But is a survivor and I think when you hear her story, you’re going to say, “Oh my gosh, how could anyone have had so many different things to deal with, especially at such a young age.” So welcome Ashley Dedmon. Thank you so much for being with us today.
Just tell us a little something about why you are a survivor, but not a survivor, but you could be a survivor. Share that with us.
Ashley: Absolutely. Dorothy first, thank you so much for this opportunity to be able to share my journey and my experience. Um, I’m a huge advocate for The Rose and the work that you and your team and your breast navigators do in the community, not only in Houston, just beyond.
And so very grateful and thankful for Um, the impact you and your team are making here in [00:02:00] our community. So to, absolutely, absolutely. So, you know, it’s a very, it’s been a very interesting road. I am an undiagnosed woman. I am a high risk woman. I carry a BRCA2 gene mutation, which makes me at a higher risk for breast cancer compared to the average woman who’s at a 12% to 13% risk over her lifetime.
And I’m gonna share more about what having a mu— a gene mutation means later. Good. But I think to your question is: I am not a survivor in the traditional sense of the conversation we’re having today, but throughout my journey, I’ve had women tell me you’re a survivor of the impact of this disease and the impact this disease has had on your family.
And [00:03:00] so when you say a survivor, but not a survivor, but a survivor, that’s really how I look at it. I’m a— I’m not a survivor in the traditional sense, but I have survived and— and thriving from what this disease took from me. And, and ultimately that was my mom.
Dorothy: So you were very young when she was diagnosed.
You, you were introduced to the breast cancer ward very early on. So how old were you when she had her diagnosis?
Ashley: So I was 18 years old when she was diagnosed with stage four or metastatic breast cancer. I knew that her mother, my grandmother, I had breast cancer, but it hadn’t really hit our house yet, our household, our address yet until my mother was diagnosed.
And we were actually on vacation, Dorothy, and we were going through our, we were going into our hotel room. And at that time, I don’t know if you [00:04:00] remember those metal plates that were on the floor of hotel rooms, um, going through the threshold and that metal plate on the door threshold was loose. And so she tripped over that metal plate on the floor and she fell. And when we got back home here to Houston, she had been complaining of back pain. And so my dad told her, let’s get you to the ER. Let’s see what’s happened. Let’s see what’s going on. And so little did we know that a emergency room visit would end up and result in a, metastatic breast cancer diagnosis.
And I remember the day the doctor told my dad, this particular doctor, not all doctors, but he came out. He said, your wife has stage four breast cancer. She has six months to live. And he walked off.[00:05:00]
Dorothy: Devastating. Oh my gosh.
Ashley: Devastating. And I was in the waiting room and I saw my dad hit the floor, hit his head, hit the wall and. kind of go down to the floor. And I’ll never forget it was in the 11 o’clock hour because Young and Restless was on. And, um, I was like, you know, that’s kind of the time correlation.
So it was like midday almost. And I remember hearing this thump and I looked around the corner and my dad had just was balled up on the floor crying because not only of the news he had just heard, but how it was delivered to him, Dorothy. Um, and, and me being a teenager in the next room overhearing this information, it not coming directly from my dad or it not coming directly from my mom, it was, it was scary.
And so life began to look different really quickly after that day. My mom was a, uh, a [00:06:00] principal. My dad was a, um, a football coach. So we’re an education family. And that’s really when the education began and learning more about this disease. And my mom started identifying her doctors and everything just moved quickly, changed quickly.
Um, and over the course of those four years, she underwent hormone therapy, chemo, and radiation. And during her, um, treatment, um, she and my dad traveled to, um, other comprehensive cancer centers outside of the Houston area to get, get some second opinions and get additional answers to some of the questions that they had had.
Um, but during that time, no one had asked my mom about her family history. No one had talked to her about genetic testing. And so, and I know had they asked those questions, my mom, being an educator, she would have come back and said, you know, “Ashley, Hey, [00:07:00] this is the information we found out. This is the information I want you to know,” because my mother was very big on empowering me and educating me.
And I even asked my dad, I said, dad, have they ever talked to y’all? Or did they ever ask mom about her family history or about genetic testing? And. He said, No, they hadn’t. And so, um, life looked really different. Um, Over the course of those four years, she went through those treatments. I was getting ready to graduate from high school.
Um, I received a volleyball scholarship to, to go off and play a collegiate volleyball and I had to leave my mother behind. That’s what it felt like. And, um, but I knew she wasn’t far. I was right up the road. I attended Prairie View A& M University, so I wasn’t far and that was very comforting. I went off to college and I want to say maybe like the second practice, second volleyball practice. I asked [00:08:00] myself, “what are you doing here? You need to be at home with your mom.” And I went over to the coach and I said, thank you for this opportunity, but I have to go. And I didn’t quit school, Dorothy, but I just said, you know what? I need the time that I do have outside of school. I need to go home and spend that time with my mom and my dad and helping, you know, be that caregiver for my mom and helping to support my dad who is caring for her.
Dorothy: And metastatic breast cancer, when we talk about that, this is a very aggressive stage in this breast cancer journey. And a lot of times, once it’s hit that, there’s just not a lot of treatments that are going to be very effective. And, you know, that is the stage we hope we never have anyone diagnosed at.
So, she didn’t even get to go through the different — you know, oh, it’s small or it’s early detection or any of that you had to face. This [00:09:00] is serious from the get go.
Ashley: Absolutely, and to your point, no breast cancer diagnosis is the same for any woman or any person and metastatic breast cancer Especially is its own disease.
We know that we’ve made a lot of advancements with metastatic breast cancer through research and science, um, but it’s still today a disease that is incurable. And so it was definitely different. Um, and I think at that time, it was really hard to accept that.
Dorothy: Well, and you’re right. No one talked about metastatic at that time.
I mean, that wasn’t even, on the horizon yet. And it’s so amazing to me how much all of that has changed in the breast cancer arena. Because now there’s, we just know, you know, we’ve got to be paying attention to all of the different stages and especially that one.
Ashley: Absolutely.
Dorothy: You’re 20- ish and she’s on her last [00:10:00] part of her journey.
And what else happened at that time? I mean this wasn’t just the only cancer that you were having to deal with?
Ashley: Absolutely. So shortly after my mom passed away, she, uh, passed away three months shy of my college graduation. And I look back and I’m so glad that I made the decision that I made because I got to have more time with her on the weekends.
I got to support my dad. I think it’s so important the role that caregivers play in the journey of a patient who’s been diagnosed with cancer or any disease. It not only impacts that patient, but it impacts their loved ones and their children, their spouses and significant others. And so, um, but during that time, while my dad was caring for her, he forgot about his health, Dorothy, his annual exams. Kind of fell by the wayside because she was his top priority. And [00:11:00] so shortly after she passed away, I got a call while I was on campus and my dad said, “Ashley, I need you to sit down.” My heart just sunk. It dropped. And I was walking across campus in front of the library. So I literally just sat on the ground.
And he said, “Ashley, Daddy has prostate cancer.” And Dorothy, I was 21 at the time. And I remember asking myself, what is going on in my family? And I really felt like cancer was coming for me. I felt like cancer was next for me and I was scared. I was terrified. I was hurt. I was still grieving. Um, I was getting ready to graduate from college and start my young adult life and career.
Um, and that again, I had to [00:12:00] pivot again, life changed, life looked different yet again. Um, but You know, it’s an honor to be able to take care of my mom and be there and take care of my dad. And so I graduated, I moved back home and, um, moved back home so I could now start taking care of my father. Um, and luckily he was able to have surgery and get his prostate removed without any additional treatment.
But I had to realize he was now going through his journey on top of grieving his wife.
Dorothy: Right.
Ashley: And so, um, I had to, I had to put me on the back burner. I was still moving forward, but I had to put me on the back burner, which I would do it again because those are my parents.
Dorothy: And isn’t this what caregivers do though?
They, everybody else becomes like that. Many times become more important and the caregiver forgets that they also need that attention.
Ashley: They do. And I think that’s what my [00:13:00] parents taught me. I knew that now that as I was caring for my dad, I had to check about my own health and understand what was happening in my family.
My dad informed me that my great great grandmother also had breast cancer. So now I’m identifying three generations of women on my mom’s side. Great grandmother, grandmother, mother, now him. And so I reached out to my OBGYN. She, I updated her on my family history because that can change annually, and that’s when she talked to me about genetic testing and genetic counseling, um, to help me to see if I was high risk for breast cancer, ovarian cancer and other cancers.
And so at the age of 21, I was tested for, um, the BRCA, uh, gene mutation. Uh, we all carry the genes.
Dorothy: Right.
Ashley: Men and women. Um, it’s genetic testing that helps you to identify if you carry the mutation. The mutation, if you are positive, [00:14:00] there’s BRCA1 and BRCA2. They both have their own individual risk for cancer. But carrying a BRCA2 mutation has my risk up to an 87 percent risk compared to the average woman who’s at a 12 to 13 percent risk over her lifetime.
So, I felt, and how I interpreted that information was, it was not a matter of if I got cancer, but a matter of when I got cancer.
Dorothy: Ashley, that had to be so hard in your early twenties to realize that you’re walking around with basically a time bomb that could go off anytime. And you’re, you really don’t have a lot of choices.
You don’t have, there’s not a medicine you can take. There’s nothing you can do. Now I want you to fast forward a little bit to when you did make such a drastic decision. About how you were going to, [00:15:00] I mean, honestly, this is handling this disease that you knew you would have your mother, you’re already a mother, and you’re married.
Ashley: Yes, yes. So in December 2016, after about 10 years of increased surveillance, which was having my baseline or my first mammogram at the age of 21, turning 22, and breast MRIs and breast ultrasounds to aggressively monitor my breast health, after about 10 years of that, um, I saw myself, Like you said, putting every, you know, as women, we put everything and everyone else ahead of our health.
And so I went back to my high risk oncologist and I wanted to explore my other risk management options. Um, and that’s when I explored and began to look at preventative procedures to drastically reduce my risk, um, for breast cancer. And so at the age of 31, after having, [00:16:00] um, My husband and I having our first child and being able to breastfeed her, I decided to have a preventative double mastectomy to reduce my risk.
And that was a very, it wasn’t an easy decision to make, but I knew my risk. That decision was based on facts. And the facts were, I had a family history. The facts were that I carry this mutation, which makes me at a higher risk. And so based on those facts, I was able to make an informed health decision.
And another thing was I had dense breast tissue, Dorothy. And so we know that dense breast tissue can put you at a higher risk.
Dorothy: And it can hide so much.
Ashley: It really can.
Dorothy: Even if you’re doing the MRIs, even if you’re doing everything, yes.
Ashley: It can. And so I think a lot of it was I was being called back to just double check.
And so I was very hypersensitive and aware, and I felt empowered by risk [00:17:00] management, my risk management options with increased surveillance. But I knew I wanted to do something more, and I had to take into account where I was in life and what life looked like. Like and what was the best decision for me and my husband, but it was also a very emotional decision, Dorothy. I was not prepared for the emotional impact of my decision. I began to question my womanhood. I began to question my femininity because I didn’t have any breast.
Dorothy: So here you are, you’re a young woman, and you know, the other risk factor you were dealing with was just having a child.
Ashley: Yes.
Dorothy: And all of those hormones that go crazy during that time.
So here you are, young woman, this was a very deliberate, thoughtful, knowledgeable decision. You made it with your husband. But then, like you said, you don’t have breasts. A prophylactic double mastectomy is a huge, huge decision to make for a young woman. And, you know, we hear of it in other situations, [00:18:00] but most what I call ordinary daily citizens just don’t even think about that.
So for you to have moved from surveillance to that, I mean, a that’s a huge step. So here you’ve had it. And I I remember hearing your story before and who you saying I started to question and I thought, Oh my gosh, she went through years of very deliberate, very thoughtful doing what you had to do. And then after it was all over, tell us a little more about how that felt.
Ashley: So I did. I questioned my femininity. Um, prior to my surgery, I, I was an A cup, you know, I was, I was not very blessed in that area. And so I remember talking with my reconstruction surgeon. Um, I had a, I have a fantastic medical team. Um, and he said, Ms. Dedman, you know, unfortunately, you know, Implants aren’t made in your [00:19:00] current size, so we’re going to have to go up a size.
And, um, I said, you know, okay. I said, as long as you, as long as I can look in proportion with my body, I will be happy. And I completely trusted him. But I think another thing was now I have bigger breasts. And so sometimes it’s like, oh, bigger, the better. And it’s not like that when you’ve been used to one size and you’re confident in one size. And now you’re having to go bigger. And that’s not necessarily a choice you would have chosen. But this is your new you. This is the new, um, your new normal. I also had to really physically rebuild my stamina after having, like you said, a major surgery like that, really rebuilding my stamina.
I love to work out and stay active. And so I had to find a new way to stay active and rebuild my stamina. Um, Um, I love to lift weights and for a while there, that’s not something that I could continue to do. And so I had to find new ways [00:20:00] to continue to lead, you know, lead and healthy and active lifestyle.
Um, and so I think what really helped me was my, my husband and my support system and my faith in God to really, Help me to know that, um, I made a decision because when I look at what this disease did it aggressively breast cancer aggressively attacked three generations in my family and the pivotal moment for me was genetic testing and counseling where myself and my girls in future generations in my family can aggressively and preemptively attack breast cancer.
And that’s how I like to look at it.
Dorothy: That’s wonderful. That is such a positive note.
Ashley: Yes.
Dorothy: And I do remember you talking about you had a young baby. Couldn’t pick her up.
Ashley: Yes.
Dorothy: And that started you on a whole, a whole different educational journey. Tell us about that.
Ashley: It did. So [00:21:00] as I was going through my, um, my recovery from my preventative double mastectomy, um, I couldn’t pick up my daughter.
I couldn’t pick her up out of the crib. I couldn’t put her in the car. And when I was able to drive. I, um, I would take her to school, but her daycare staff would have to come and lift her out of the car and I hadn’t returned to work yet. So my day, my activity would be drop her off at school, come home and rest, go pick her up and then come home and rest.
But it was really hard to articulate to her why mommy couldn’t do all of these things. And so as I was in that recovery phase, I thought about, conversations my mom and I had had about the hardest part of her breast cancer journey. And she would share with me, “Ashley, the hardest part was letting it— was telling you that I was diagnosed. It was not having the words to share. It was not knowing what information to tell you and when and how.” [00:22:00] And I even thought about my time as a teacher when I would have students come and tell me that their mom was diagnosed, their aunt was diagnosed. Um, and you never know when our children are going to hear this information.
They could, Their first information about breast cancer could be from a friend or, you know, at school. And so, I knew that I wanted, I was looking for some tools and resources to help me to have a conversation with my daughter. Again, undiagnosed, but I had had a procedure that is, that aligns with a woman who, who is diagnosed.
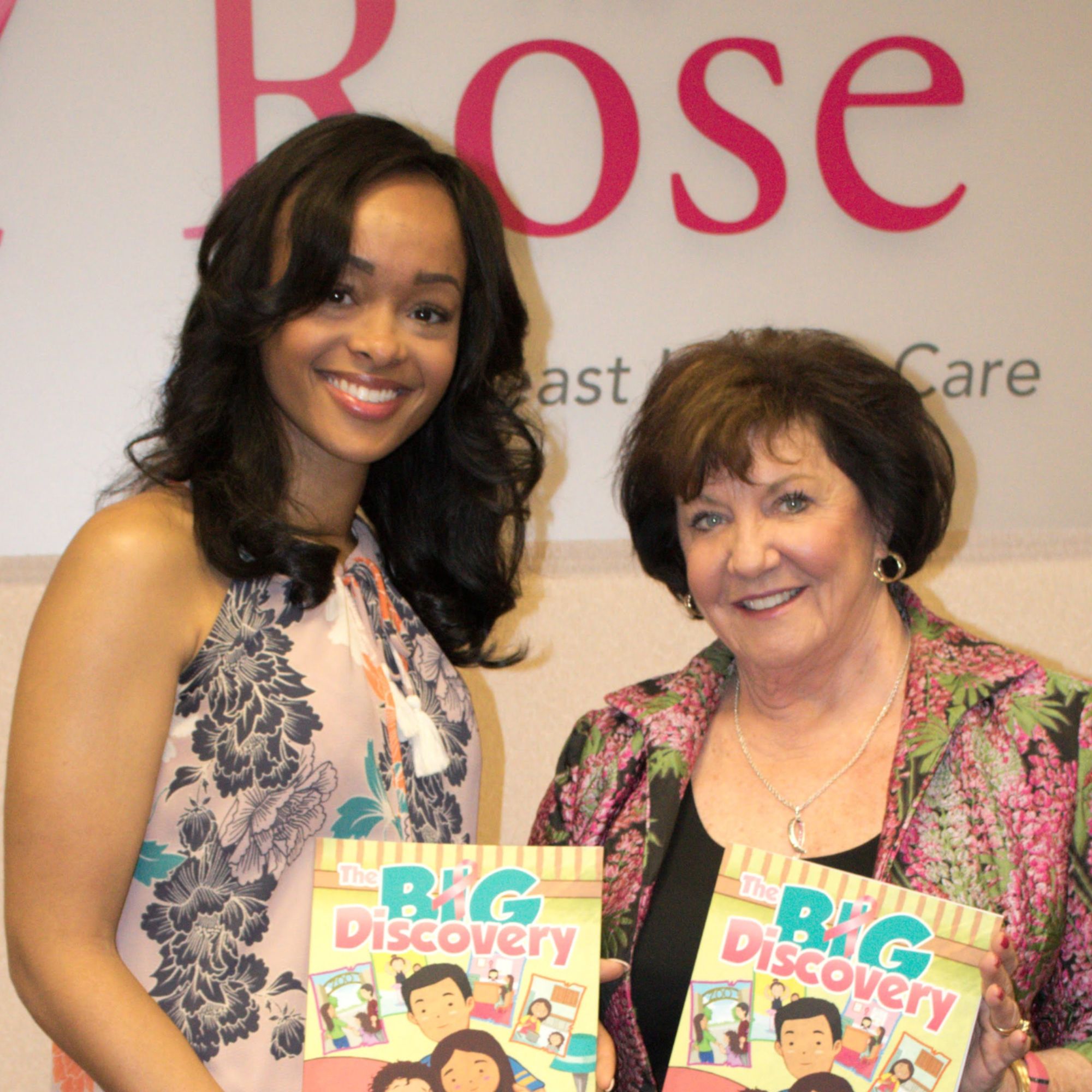
And so there was not a resource out there. And so I just said, you know what? I’m a teacher. This is what I do. Let me create a resource. And so that’s what I did. I wrote the big discovery.
Dorothy: And let me tell you, it’s an excellent resource for Children. We keep it in our navigation department because you’re right.
Children only hear mama sick. They don’t hear [00:23:00] All the other things and that almost always equates to something bad is happening and somehow I caused it.
Ashley: Yes.
Dorothy: Or somehow I did something bad to bring it on. So it’s a excellent book, excellent resource. You’re republishing it.
Ashley: I am. So ultimately, the goal of the book is to serve as a educational tool to assist families and their children to navigate through a breast cancer diagnosis.
It helps to facilitate, like you said, difficult conversations a mother could have with her child to really help them understand the importance of early detection. Um, and the diagnosis of breast cancer. Um, one thing that I was very strategic about was the treatment process is introduced in the book, but it’s left open because Everyone’s treatment, everyone’s diagnosis is different and everyone’s treatment plan is different, but it’s really helped really positioned to help start the [00:24:00] conversation with families.
Um, and, and because again, I’m undiagnosed. At the back of the book, there are 10 stories from diagnosed women who have had to tell their children. And so those women are talking to the mother that’s reading the book and encouraging them and sharing how they told their children. This year, I’ve received a lot of great feedback with The Big Discovery.
Um, but this year I’m actually going to republish with Um, right now, the characters are characters of color, and I’m planning to republish with African American characters. And the reason behind that is black women are 40 percent more likely to die from breast cancer than our white counterparts. And there’s a lot of disparities in the black community in communities of color.
And I wanted to be able to provide a resource that really targets and nurtures the different challenges that women of color face and [00:25:00] to really help to target the same goal and purpose of the book in a more targeted and strategic way.
Dorothy: Let’s stay with your community for just a minute. Do black women have any difficulty talking about mammograms or, you know, I’ve heard different stories. Sometimes it’s just, well, we don’t talk about our health. Sometimes we’ve got too many other things to have on our mind. We’ve— You know, so what have you seen different in the black community when it comes to breast cancer, mammograms, taking care of yourself?
Ashley: That’s a great question. I think, well, first I’ll say this, I think as women in general, we, you know, we’re, We’re, uh, balancing work and home and children and life and family and things that we’re engaged in.
Um, so I think that’s, you know, women in general, whether they be white, black, Hispanic, Asian. Um, I think, and, and I can, I can speak for me, I can’t, you know, it’s, I don’t wanna speak for the entire, [00:26:00] um, black community, but what I will say is that as we are entering into the health care system and we’re going through that continuum, it does look and it can and it has in the past look different for black women and women of color.
Um, access to mammograms and high quality screening is a barrier for us. And when I think about the mission of The Rose, that’s what you and your team provide not to all women, white women, Hispanic women, black women. And so it’s, it’s services that The Rose provides with high quality mammography screening. That is something that traditionally we don’t have access to in the black community. It’s, um, also those social factors. that impact health outcomes in black communities and communities of color and in any other under supported communities. Um, [00:27:00] and it’s also navigating through racism and bias and micro aggressions when, when we are in the healthcare system.
So there are different challenges and obstacles that we have to, um, Navigate through and I don’t even want to use the navigate the word navigate because we shouldn’t have to you should navigate through those, uh, those things, but we do. And it makes it very harder to be able to, um, to access care. And we know that that can lead to more aggressive forms of breast cancer; more pro— you know, um, to later stages of a diagnosis. And so not necessarily aggressive forms, but just later stages of breast cancer because of those, uh, factors.
Dorothy: And you’ve touched upon so many things. The, the social impact. So many times we hear that in, especially in unsupported [00:28:00] communities, it is that support that women lack and they don’t know where to go and they, they don’t know who to talk to.
The access to care is a huge issue. Huge. And the, the problem that I see is it’s like even if they knew of an area to go to, it’s like they’re still going to end up last on the list. You know, it’s like, oh, that’s going to take time, that’s going to take this, that’s going to take that. Like you said, that’s not unique to black women.
But, boy, considering that you could very easily have a much more aggressive cancer. And triple negative that shows up so much more often. I think I think one of the the problems I have with our screening Recommendations is that we really haven’t taken in what happens to the black woman the young black woman we our united states preventive task force says Start at 40 because [00:29:00] that’s, you know, you don’t magically change overnight when you’re 40.
But for our young women, they hear, “Oh, you need to go get this done.” And then when they try to go get it done, it’s going to turn out to be a diagnostic mammogram because it’s not, she’s too young for a screener. And so she’s going to pay more. It’s kind of like we’re penalizing her all over again. Yeah.
And I just, that just drives me crazy. So you’ve always been a teacher. I mean, The teaching family, you’ve been, that is part of you, but you’ve really, your history has now moved your career in a very different way.
Ashley: It has, you know, I call it, you know, my purposeful work. And, um, and to your point, your last point, you know, black women are being diagnosed younger and with more aggressive and advanced stages of, um, of breast cancer. And so education has been something again, that has been embedded in our family from both of my [00:30:00] parents to myself. And so I, I try to stay a student of this work and of the science and the technology. And we’ve made so many advancements through science and research. And along the way, I’ve been able to really position my purposeful work, um, and even professional work towards learning more about this horrific disease, and I’ve been able to work at the local, state and national and global level with different organizations and nonprofits to be able to first, Dorothy, educate myself; to be informed about the work that I’m so passionate about. I’ve gone through a patient navigation training at GW so that even when I’m having just conversations at the grocery store on the phone, I can kind of step outside of my own experience and really look at what the person is telling me and really help to to [00:31:00] guide them to resources, community health workers, The Rose. asking for a breast navigator. Um, so that some, there is someone that can help to, um, guide them through the process.
And so I’ve been able to work with, like I said, with several organizations to be able to, um, advocate for, for the importance of, uh, knowing family history and genetic testing. I know a few that I work for our force. Um, facing our risk, uh, cancer empowered where I serve as a peer navigator to help guide other women through their journey.
Um, working with Tiger Lily and the great work that they’re doing with addressing, uh, health disparities in black and brown communities. Um, I also, uh, work, uh, as a, um, a volunteer with, um, the Basser Center for BRCA on their, uh, black and BRCA initiative, really talking [00:32:00] about the importance of genetic testing in the black community.
And there’s several others that I volunteer with, um, to be able to give back, Dorothy, because we have to go back and share this information that we’ve learned to help others. And I like to think of it as my mom was an educator, and I don’t want her journey to be in vain. I want to be able to share it with others.
And it’s been great to partner with these organizations that have equipped me and educated me, um, and to tell my journey and to help other women. be able to feel empowered to do the same.
Dorothy: And so you’ve touched upon genetic testing and the genetic counseling is equally important because we could hear a whole lot of things and and get it in our mind that this means this but I know that that you had a great counselor you had someone who really knew what they were doing and again that is fairly new in, in our breast cancer arena, I, I think, and I’m going to [00:33:00] encourage all of our listeners to go and find your TED talk. We’ll put it in our, our link because you really go into here’s what it meant. Here’s how I handled it. Here are some of the things that I didn’t know to ask and learned, you know, so I think anyone that is even thinking about it should really go listen to that TED talk.
And I know you have a lot of resources that you could direct people to.
Ashley: Absolutely.
Dorothy: So do you still have a yearly checkup?
Ashley: That’s a great question. My risk management has looked different over the last now decade plus. So as I shared earlier, when I was 21, I started, um, I had my first mammogram. Had breast MRIs and breast ultrasounds to aggressively monitor my breast health.
Now that I’ve had the preventative mastectomy guidelines, state that I no longer need to have a mammogram. I still see my high risk oncologist and my surgical oncologist once a year for clinical [00:34:00] exam. And Dorothy, I practice myself breast awareness every day. And that awareness is looking and seeing and smelling and just visually aware of my breast and any changes.
Um, because that’s first, I know my girls are also watching. And so I still have to practice, um, just that self awareness, not only for my breasts, but just for my body as a whole. I still do have my ovaries, even though my husband and I are finished with Um, with our family planning, I still see my regular OB annually for my well woman exam, but I also see an oncologist, gynecologist for my CA 125 blood work and transvaginal ultrasounds, which still monitor, um, my my ovarian health.
And as I approach 40, I will consider a Salpingo-oophorectomy, which will help me to further reduce my risk [00:35:00] for ovarian cancer.
Dorothy: Well, you’ve certainly taken all the right steps in keeping yourself healthy. Now I have two more questions. You know, your mom put everyone else ahead of her own health. What would you say to her today?
Ashley: I think if you would have asked me this question when I was 21, and you referenced my TED Talk, um, and I start off that TED Talk with a strong statement.
Dorothy: Oh, yes.
Ashley: And that statement is, “I hated her.” And when I was 21, I probably I had those feelings and I didn’t hate her. It was the feelings that you go through when you go through grief and of losing someone. And it was my mom left me and I hated the fact that she left me when I needed her the most. Um, and now that I’m, I think I’m 36 or 3—, I’m 37. I’m like, how old am I? Uh, now that I’m 37 and I’ve experienced life and I’m a wife and I’m a [00:36:00] mom and I’ve been in this space for so long, I would thank her because I believe that She made the ultimate sacrifice.
And I think when you think about moms and parents, that’s what we do. And I think if my mom knew someone said, you know what, you have to go through breast cancer so that your daughter can find out this. And your grandchildren can do this, I think she would say, sign me up.
Dorothy: Oh, Ashley, that’s beautiful.
Ashley: And because I think that’s what mothers do, we, we sacrifice.
And if it means we have to take on things so that our children and our grandchildren don’t, we, we wear that, we take that on. And so I think she would do it all over again. And I think that’s what her lesson has taught me. It taught me to be an advocate for my health. It, it, it prompted me to go out and ask questions about my own health and advocate for my health.
And so, Her sacrifice [00:37:00] has helped save generations to come. I shared this a couple of weeks ago with someone else. My results that I received from my genetic testing, um, from the lab, I’ve put in my living will. So that if something were to happen to me today, when my girls who are now three and eight get older, they may not remember the conversation.
But when they go for, their doctor’s visit and talking about their family history,
they have my report that shows that I carry this mutation, that my mom was high risk. This is my family history, so that they’re standard, so that they’re able to navigate through their journey a little bit more easily. So I would thank my mom because she has given me And her two sweet baby granddaughters, a gift of knowledge.
Dorothy: And that is an excellent, excellent idea. My goodness. You can’t make it any more clear than what you’ve done.
Ashley: Yes.
Dorothy: Ashley, one last question. What are [00:38:00] your dreams for your daughters?
Ashley: I want my girls to know and understand their family history of cancer, which is a conversation we have very early. They know why Grandma Lynn died.
Um, I want them to know and understand my risk for breast cancer, ovarian cancer, and elevated risk for other cancers. Um, my oldest daughter knows that I carry a BRCA2 gene mutation. We kind of joke about it. She’s like, you’re a mutant mom, you know, because when they hear that term, you know, their mind and creativity just starts going.
Um, but I hope that neither of them have inherited this mutation. They have a 50, 50 percent chance of inheriting my mutation. We get half our DNA from mom, half from dad, either both of them have it, neither of them have it, or one of them will have it, but I want them to understand either way, um, what regardless what their risk is [00:39:00] based on their family history.
I want to equip them with the tools and resources to make informed health decisions and empower them to advocate for others and advocate as they navigate their own health. Um, not just with their breast health, but also their mental health, their heart health, their maternal health, whatever it may be.
That’s really my goal for my girls. I want them to be able to pass this information on to their Children and their Children’s Children because I believe through the gift of knowledge that we can change an entire generation from being impacted by this horrific disease.
Dorothy: Well, it’s a great dream. I certainly hope that it comes true and we know that if you’re behind it, it has a great chance of doing that.
Ashley: Thank you. Thank you.
Dorothy: So. Ashley, advocate, teacher, mother, wife, thank you so much for being with us today and for sharing this story and, [00:40:00] and who knows, you may give another young woman that courage to say, I’m going to take these matters into my own hands and I’m going to do something to change my future.
Thank you again so much for being with us.
Ashley: And thank you, Dorothy. I appreciate you and everything that you and your team do here at The Rose. And again, just the impact that you’re making in the lives that you’re changing and saving through your work and your mission.
Post-Credits: Thank you for joining us today on Let’s Talk About Your Breasts.
This podcast is produced by Freddie Cruz Creative Works, and brought to you by The Rose. Visit TheRose.Org to learn more about our organization. Subscribe to our podcast, share episodes with friends, and join the conversation on social media using the #Let’sTalkAboutYourBreasts. We welcome your feedback and suggestions. Consider supporting The Rose. Your gift can make the difference to a person in need. And remember self care is not selfish. It’s [00:41:00] essential.