Dorothy: [00:00:00] Imagine being uninsured, working in a low paying job, and hearing the doctor say you have breast cancer. First question in your mind is going to be, how am I going to pay for this? Well, The Rose’s Navigation Program is here for that very reason. And the two women we’re talking to today have the answers for every question that patient has.
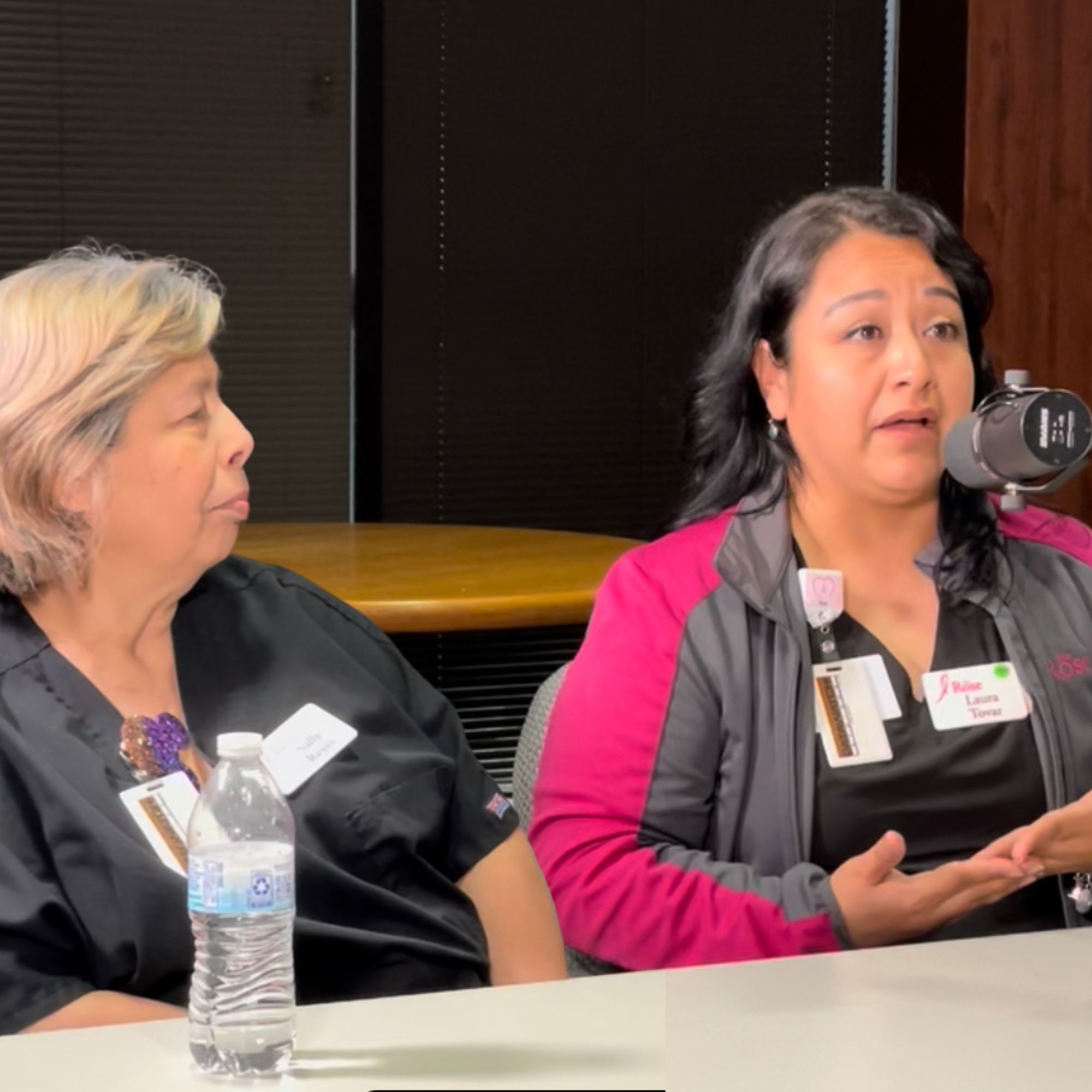
At The Rose, we know these women as Laura and Sally. Our patients call them angels.
Let’s Talk About Your Breast. A different kind of podcast presented to you by The Rose. The Breast Center of Excellence and a Texas treasure. You’re going to hear frank discussions about tough topics. And you’re going to learn why knowing about your breast could save your life. Join us as we hear another story and we answer those tough questions that you may have.
Hi, I’m Dorothy [00:01:00] Gibbons and I am the CEO and co founder of The Rose, Breast Imaging Center of Excellence. And today we are going to talk about patient navigation. Now, this is a term that you may hear a lot, but at The Rose, it has a little different meaning, a little different process. And I want to tell you how this got started.
We were very much involved with mammograms and ultrasounds we were diagnosing women. And, and in my naivety, I thought all we had to do was: send a woman with her slides, with her results, to whatever doctor or hospital would be taking them, and she would just get right on in and get her treatment, and all would be well.
I soon learned that so many of our patients were turned away at places. Not for anything they did or not, not because they hadn’t filled out the paperwork or they hadn’t done the application, but they missed one little thing on it and then they [00:02:00] would get turned away. And then I, I started saying, well, this isn’t right.
This woman has breast cancer. I mean, we know she has breast cancer. We’ve got a diagnosis. And it was always the same story. The woman would stand in line and then she’d find out she needed something else and then she’d be turned away. And these are people that don’t have that kind of time to be waiting day after day after day to get into a system. So we started Patient Navigation, and its whole purpose was to be someone to walk with that woman from the time she was diagnosed, to the time she got into treatment, and then beyond. I think of all the programs we have at The Rose, this is by far the one that is our mission.
It is what we promise our patients. It’s what we promise our community, we’re not going to leave you alone. We’re not going to let you go off on your own and find something. We’re going to be there and we’re going to keep working until we do. [00:03:00] And in the beginning, when we didn’t have really good processes, so state processes for getting women into treatment, we had to rely on our physician network.
And it started with one doctor and then two doctors. Before we knew it, we had 500 doctors willing to provide one service a year to a woman and most of them gave a lot more than that. But just to help get her through— it would be a surgery, it would be chemotherapy, it would be radiation therapy, whatever it took.
And at that point, our navigators were not only just getting them through a treatment, but also trying to organize and set up all those different appointments. So today we have two out of our three navigators. Sally Reyes has been with us since 2008. Welcome Sally.
Sally: Thank you.
Dorothy: And Laura Tovar has been with us since 2012.
Laura: Thank you for having us.
Dorothy: Sure, sure. So I know that being a patient navigator takes a different kind of mentality. [00:04:00] At the end of the day, you’re handling and being with women at the most vulnerable times of their life. And so our navigators are actually in the room when the woman receives the diagnosis.
And we have the doctor, the patient, maybe a caregiver, the navigator, and that patient is thinking a hundred different things. But we all know that when you hear you have breast cancer, your whole reasoning goes out the window. All you can think about is, am I going to live? And for uninsured women, they all, what you’ve told me is, they always say, “how am I going to pay for this?”
So, Laura, what is the most difficult thing in your job? Is it being in the room at that time, or is it when you’re trying to explain, “here’s what you’re going to have to do to get treatment?”
Laura: The hardest thing is speaking with the patient regarding their [00:05:00] treatment process. But most of the time when you’re diagnosing them, the first thing that comes to their mind is “how am I going to pay for this? What am I going to do? What about my Children? What about my family?” So we try to give them some peace before leaving at— in finding them treatment, a way to get their treatment, because this is what we’re here for to help them get that treatment. So whenever they’re worried about what’s going to happen, their first thing, like I said, is how am I going to pay for this?
So we obviously try to assist them with trying to get their treatment started. Whether it be helping them apply for Medicaid or any type of program that is available for them to get their treatment started.
Dorothy: And before they ever get to your office, you pretty much know because of their paperwork, because of the information they’ve already given us, which program is going to work for them?
Laura: Correct. Yes. So as soon as we get that message that this patient is a positive patient, we [00:06:00] immediately start looking into her information and to see what this patient would qualify for. So, that is why we use the financial assistance application and we go based on that. Of course, sometimes we don’t have all the information on that application. So when they come in, we do have to speak with them to see what would be the best option for that patient.
Dorothy: Right. And there’s so many different programs that we do have. Not enough. Never enough. But it, it, each of them has a different criteria. For some, you have to be 200 percent poverty level. And that poverty level is determined by your entire household income. Is that correct?
Laura: Yes.
Dorothy: Yes. And that means if you have two or three people in the household and your teenage son is working at the local hamburger place, that income is going to count too. And you know, that’s one of the things we can’t change some things with our programs, but we certainly have to be aware. We don’t want her to get on down the road and [00:07:00] then be denied.
Laura: Correct. Yes, we do inform them of that. We do have those three programs that are available. We do have to, like I said, when we review the financial assistance application, we do determine what would be the best option for her.
Of course, we always hope that Medicaid would be the first option because it is a Uh, faster process sometimes, and it’s easier for us to get them into treatment. Unfortunately, not all our patients qualify for Medicaid, and this is why we have to go a different route. But sometimes those routes take a little bit longer for those patients to get into treatment, and that is where we are having issues with, you know, getting them in quick, quickly, which Sometimes it’s not necessary that they have to be seen right away, but of course, with our patients being worried and having this thought in their head that, you know, something’s wrong with me. I need to get treated [00:08:00] quickly. We understand the urgency of the matter. So we try to do as much as we can. But sometimes with the other options that we have, it’s out of our control and we can’t do—
Dorothy: And so some of what you’re doing then is just helping her, calming her down, talking to her, checking in with her, and saying we’re still in process.
Laura: Right.
Dorothy: But like you said, they know something’s wrong and suddenly they want it done, they want it out, they want it, yes.
Laura: Yes.
Dorothy: They want to take care of it. So Sally, I know that part of your job is to follow up with the patients after we’ve got him into treatment. And when you call, what kind of questions are you asking?
Sally: See how the treatment’s going, if they’re doing chemo or radiation or how’s their family doing with them because it affects the kids. The husband, it affects, it affects all of them. So I want to know, do [00:09:00] you need food resources? Rent resources? Because it takes two now to work.
Dorothy: And what you’re saying is when people are in treatment and they’re used to having that income coming in, you know, because they’re the second person working in the house, then suddenly they may not have that income.
Sally: Or they’re single moms.
Dorothy: Oh yeah.
Sally: That don’t have other options for that too. And they need a lot of resources. And that’s what we, we come in and look at the resources we have. And we start calling people. Also, we provide wigs and prosthesis with them while they’re getting treatment. when they have surgery and it depends on what they’re going to do.
Dorothy: I’ve heard you tell these stories about how a woman comes in and she’s, she’s had a mastectomy. She doesn’t have prosthesis, which are not always something we can find, right? I mean, they’re not in the insurance or in the Medicaid process that don’t always happen like that. So we have some. So tell me [00:10:00] what happens when you fit a person.
Sally: I measured them and I tell them different sizes and we go to different bras and prosthesis and I love the look when they have that, “wow, I look wonderful.” I, they put on the blouse and it makes my day because it’s like a whole new person. And then with the wigs too, I style it with them. I help them. I’m like, look, you can be blonde today. You can be redhead tomorrow. You can be a different, a different person. And It makes them feel good. It makes me feel good that I’m helping them to feel better and look better because we all women want to look good.
Dorothy: Absolutely.
Sally: And it’s just them putting I had a lady that was going to go to her wedding, And she said “I have to go to my daughter’s wedding, but I have, I have only half, I mean,” so I said, “no, we’re, I’m working to do a nice bra with the prosthesis and we got her a lacy one.”
So [00:11:00] pretty. And she was just, it light up. It, it made my day. For everything else, it’s just looking at her to make her happy. And she was going to look beautiful. I mean, she was beautiful already, but she was going to have that confidence walking her daughter on her wedding day. That was priceless. Nobody can ever take that away from her, from me, because I can see her actually walking down the aisle with her daughter. And that’s one of the—
Dorothy: That is a beautiful story. Thank you. We have people in tears here and, uh, but it is a beautiful story. So Laura, when you’re trying to get people into treatment, do you, do you help them also to understand what the treatment involves?
I mean, um, if it’s chemo or surgery or—
Laura: Part of the patient navigation consultation is obtaining the results from the doctor, either Dr. Melillo or Dr. [00:12:00] Raz. Um, they would provide the results. And what we do is we sit there throughout that conversation. Once the doctor has completed their consult and the patient has asked the questions that she’s needed, the doctor steps out.
So we stay in there with the patient, explaining them the process. We give them a little bit more explanation regarding their diagnosis. And, you know, we have a picture where we’re showing them, this is where it’s located, this is the breast. You know, explaining them a little bit more so they can understand it a little clearer because not everybody knows the anatomy of a breast. So when we’re explaining it to them, I feel like it calms them down a little bit more knowing exactly what’s going on. And we also educate them as to the possible treatment options that they may have. The treatment options are usually surgery, radiation, or chemotherapy.
But we always do inform them that it could either be one, two, or a possibility a combination of all [00:13:00] three. But those are the questions we help them come up with questions as to what you may want to ask the oncologist because a lot of times they do have those questions as to how, how long is my treatment going to happen?
How, you know, am I going to be okay? Is my surgery going to be something quick? Is it going to be difficult for me? And those are questions that we unfortunately cannot answer because we don’t know the type of surgery that you’re going to need. But we do have, we do let them know: after the surgery, you need a prosthesis or you need a bra, you know, we can assist you with that. We can help you with what we have here. Um, but most of the time we do explain to them regarding the, the, um, treatment possibilities that they can have. So I feel like when they leave here, they leave, yes, they’re still scared. That’s something that we can’t take away. I mean, they’re going to be scared and that’s, their right. And we [00:14:00] can’t take that away, but we can at least give them a little bit more information to, for them to fully understand what’s going on, or at least kind of get an idea of what’s happening. So whenever they get to their oncologist or whenever they talk to their family member, they can give them the information and just know at the moment, this is my diagnosis.
That’s all we know. We have to wait until the next step, but at least to let them know it’s gonna be okay. I’m covered I’m gonna be able to get my treatment done. So that’s that’s what we’re here for We’re here to help them get that treatment process started.
Dorothy: And so we truly believe around here that knowledge is real important.
Laura: Yes.
Dorothy: You know women are not stupid. We can understand what’s going on. We can find a way to get through it. And many times though, some of these words they’ve never heard before.
Laura: Right.
Dorothy: So it’s not only saying you may have this or this. You have [00:15:00] to go kind of in detail talking about here’s what happens during chemotherapy. And I think it’s important, something you said about giving them questions that they may want to ask. Uh, and encouraging that, because when we get in front of doctors, most of the time our brains go, “nope,” and, and we think, “oh, I should have asked him that.” Sometimes you send them with, uh, questions to take with them.
Laura: With questions to ask. Um, usually whenever the consult is happening, they’ll have their questions already, like, you know, like I said, “how long is my treatment going to be?”
What am I going to need chemotherapy? Is my hair going to fall out? So these are questions that we don’t know if you’re going to need chemotherapy. So what happens is we try to explain to them. This is the process regarding the The treatment possibilities. Chemotherapy, if it is needed, you know, it’s a possibility because the question is, how long is that going to be for?
That depends on the treat, on the treatment that you’re needing. If [00:16:00] you’re needing chemotherapy, you know, depending on how strong that medication is needed, it could be once a week, it could be once every two weeks or once every three weeks. So this is information kind of just to help them know, kind of like a timeline. Or with radiation. Radiation is on a daily basis and it could be up to six weeks. We’re talking about 30 days, Monday through Friday. So this is something that they’re kind of like, “okay, radiation, I don’t know, but they told me it’s going to be daily. So I’m going to have to try to figure out what I can do.” So what we’re, you know, that’s the information that we’re trying to give them. So that way they kind of understand what’s going on and how to proceed with the questions to ask the oncologist because this way they can ask, okay, is it gonna be once a week? Is it gonna be once every three weeks? Because The Rose told me it might be like this or it might be like that, you know? So, um, That’s usually what we try to [00:17:00] do with our consultations and, um, but we also do speak with them afterwards after they speak with the oncologist to ask them, you know, did you ask them the question? Did you, you know, this is how you’re going to get to control your, your path, your treatment because, um, um, The more information, you know, the better that way. You’re not wondering, I don’t know what they’re going to do to me tomorrow. I have an exam tomorrow, but I don’t know what it is. Ask them. This way you can have that information and you know why they’re doing the exam. If they know this, that’s how they’re going to let me know what treatment I need. If I, if the results come back like this, they told me I’m going to do that. That’s information. And that kind of puts your mind more at ease instead of, I don’t know what’s going to happen to me.
Dorothy: Y’all never brag about this, but I hear from our physicians that The Rose patients when they come in, they are more informed than most of their [00:18:00] patients, whether they’re insured or uninsured. And that’s just that’s really a tribute to both of you for making sure they know what’s best for what’s ahead of them. And that makes me so proud. I want to be sure our listeners realize we’re talking about uninsured women. We’re talking about women that don’t have physicians, women who don’t have resources, and many of our women, uh, Spanish is their first language, right?
Laura: Yes.
Dorothy: So, you know, all of our navigators are able to speak to our patients in their language, and I, and I, I think that also lends to some of that level of confidence for them. You know, they can ask the questions in their own language and you can respond to it. But I also think knowing that you two have been so involved in patients, you have a sense for when a patient needs something else. I mean, you, you know that they may need that call the next day, even if they’re not going to call you.
And of course [00:19:00] you, you’ve had some pretty interesting spouses and children that you’ve had to deal with because they’re, tell us that story about how scared that one husband was.
Laura: I did receive a call from one of the husbands and he was upset because he wanted his wife to be seen as soon as possible. And like I said, once you’re diagnosed, everything is urgent. We have to be seen as soon as possible, which is understandable. Unfortunately, with the process of obtaining that treatment, it’s— We can’t say how long this process is going to take. We try to do our best to get you in as soon as possible. But in this case, the patient, uh, the patient’s husband did call me and he was upset that she wasn’t, um, seen right away.
And he didn’t understand what was going on. And he did get kind of loud, but like I was telling Sally that I understand why he [00:20:00] feels this way, and it’s understandable to know that in a couple, the husband is the Mr. Fix It All. Right? Anything happens, he’s going to take care of it, and he’s going to fix it.
Which is usually the normal thing for a couple sometimes. So what happened is that, He was frustrated that she wasn’t seen quickly and he could not fix it and he wasn’t able to fix it.
Dorothy: Right.
Laura: So after everything that he was telling me, you know, I told him, okay, I figured out what the issue was. I called him back and I explained to him, I spoke to them, this is what’s going to happen. We’ve taken care of it. They’re going to see her. And at the end he apologized to me and he said. “I’m sorry for the way that I’m speaking to you. I’m just, you know, I’m frustrated.” And I told him, “I understand. I understand that this is your [00:21:00] wife and she’s very important to you. And you’re gonna try to do everything that you can to get her seen. And that’s understandable.” I was like, “I know that you’re frustrated because you don’t know what to do. And it’s okay. You’re here for her and that’s what she needs. She needs that support.” So when I explained that to him, he was like, “yes, yes. Thank you.”
Dorothy: And of course he was calling the hospital that you’d already called, that you had already talked to the people in a meeting and they were, it was underway, but he wasn’t getting, of course, the answers.
Laura: He wanted the answer that he wanted. Yes.
Dorothy: Yes. And I, I, I know that had to be. For you to have stayed calm, had to, had to take some patience, but you’ve certainly had lots of experience with that, especially with family members that are worried.
Laura: Yes.
Dorothy: So Sally, can you tell us a story of the children and how important it is to include them [00:22:00] in, maybe not all the details, but helping them to understand. And I remember that one story about trying to explain what chemo was going to do.
Sally: Yes, it’s I had to think like I was a child to simplify that his mom was gonna be okay. Yes, her hair was gonna fall off. And then I showed them the wigs, I showed them the wigs that this could happen. Yes, she might be sick for a little while, but the chemo, the medicine was going to help his, her— mom go through this.
And there were certain things she could do, like, like pick up the trash or do his bed. Simple things that, I mean, even a four year old, like, Give him, give her some water. You can give your mom some water. She needs it or just give her a hug and things like that. And it was explaining to them that his mom was going to be okay.
That this was gonna pass and all he had to do [00:23:00] is smile and be, not be a good little boy, but do stuff like for her.
Dorothy: Yeah, love her.
Sally: Love her. And just smile at her and hug her and be that little boy that, oh, I’m gonna tear up. It’s so hard, I think, on the kids because it’s, they don’t want to lose their mom.
Dorothy: Right. And that’s what they hear. They hear that, oh, she’s got cancer. She’s going to die. You know, children can be so, uh, not unkind, but so candid when they hear that. And I think they also, and y’all correct me if I’m wrong, but I’ve heard y’all say that they sometimes feel like they did something wrong to bring this on.
Sally: “Were they bad?”
Dorothy: Yeah, and you’re, you know, You’re having to say to them, no, this, this isn’t what happens. I know you have some resources for Children to give them, but there’s never enough of those either. We need lots of different ways to show different Children. [00:24:00] I remember the one story where you, you, you or, Elizabeth was saying, you know, “Now, when her hair falls out, that means the chemotherapy is working. the medicine is working.” And the little boy called y’all and said, the medicine is working, the medicine is working. You know, because her hair had all fallen out that morning.
Sally: “She’s bald. But she looks pretty.”
Dorothy: Aw.
Sally: Because the mom was like my hair fell off, you know, and I look awful and the little boy’s like “no mom You look you’re the most beautiful woman in the world. You’re my beautiful mom” and Things like that that it just the little innocent little boy that does that to his mom for sure little boy little girl loves their mom so much.
Dorothy: Oh, yes.
Laura: We once had this 80 year old patient who came from out of the country, her daughter brought her in and, uh, apparently she was diagnosed and needed surgery in 2019 and they were sending money to her country [00:25:00] to get this treatment done.
You know, back in her country, they did surgeries and she was still having issues. They didn’t know what was going on. So when we asked a few more questions about it, um, You know, Sally tried to help her get gold card, but they denied her apparently because now she wasn’t here long enough as a resident. And I was like, what do they mean? She lives in Harris County. But what they were really saying was She hasn’t been here in the United States long enough. So we went ahead and tried to refer her to Methodist Charity Care. So after I was talking to the daughter, you know, getting a little bit more information, I was like, so what happened?
And oh, well, it’s because back in her, you know, in the country, something was wrong. They needed to do surgery. We all sent money over there for her to get her surgery done. She had it done. But then, you know, she’s needing more and more. And a family member was taking care of her in her country. [00:26:00] And that family member was calling and asking for more money because her her kids were here.
So they were sending money home for her to have her surgeries done. It happened maybe three times that they were sending money over. Well, the patient never had anything done.
Dorothy: They were just being told that.
Laura: They were just asking them for money. The money was being sent over and the patient was not being seen.
She wasn’t being taken care of when we saw her reports. I believe it was 2019 and she was here. She was diagnosed in 2019 with DCIS.
Dorothy: Oh, my gosh.
Laura: So what we did is we referred her over to Methodist and they’re taking care of her now.
Dorothy: Wow. All those years that she thought she was getting treatment.
Yeah, wow.
Laura: It was the worst thing. She was like, just looking at her. It was like the light from her eyes was gone. She was just, [00:27:00] and her daughter just, she started crying and we started crying. We were like, Sally left the room and I was like, okay, all right. What happened happened. Let’s proceed. Don’t worry.
We’re going to try to see what we can do. We’re going to get you into treatment and you’re going to get what you need done. And she was like, okay. And when we talked to her, her daughter, her daughter was— she was like, “Oh my God, thank you so much. She’s been taken care of. They’re working with her. She is just as happy as can be” because she would tell us that her mom wouldn’t even look in the mirror, that they had the mirrors covered because her mom did not want to look at herself in the mirror because she just, she said it was, she was ugly and she didn’t want to see it.
80 years old.
Dorothy: Well, once again, another story of someone who has been led to The Rose, found these wonderful women, [00:28:00] and y’all helped her get into treatment, so again, thank you. And I’m so glad that we do have some resources for them and that they are easy calling you. And, you know, when you were talking resources, I want to stay on that just a minute. It could be rent. It could be food. It could be gas cards. It could be many times we have had the hospitals or the physicians say, well, your patient didn’t come in today only to find out they had run out of gas or they didn’t have a ride. So some of those things you can ward off by just being sure that, that they do have them, but we have no idea how, you know, cancer is expensive.
Whether you have insurance or not, it is expensive, and so many of our patients simply do not have the financial means to do the things they need to do to get through this process. So we do have some resources, again never enough, but some [00:29:00] that we can offer. Now I’m going to ask you two, both of you, a very serious question.
And I, and Sally, we’ll start with you. So, you’re sitting with someone, they’re upset, they’re crying, they’re scared. You’re watching the family also be very scared. You’re trying to stay up and stay positive. So how do you take care of Sally at the end of the day?
Sally: I’m just so grateful for my family. My kids are in the military and I always pray that God always keeps them safe.
And I want to do the same thing for our women that come through here because it’s about taking care of everybody but also take care of me. You know, I talk to my husband, the dogs, especially God. Now, like, please God give me the strength to be able, in the worst, to help this patient go through this because It could be one of us.
And that’s what is important about taking care of each other. And we all take care of each [00:30:00] other. We, we cry about our patients. But the thing is that. We do our best to take care of each other and our families too. Because if we, women always do everything last. We have to come first to be able to take care of everybody.
So that’s the most important part that we tell patients. To going through chemo, you going through this, you have to come first. You, maybe the house is dirty, it’s okay. It might not be dirty to me. But to the person it is, you have to let things go and be good to yourself, because your child, no matter how old they are, you always need your mom and dad.
And that’s why it’s about, about empowering women, about taking care of each other now. Because if you don’t, they’re not gonna have a mom. And that’s the saddest thing. I don’t care how old you are. You need your mom.
Dorothy: So Laura, I know this is something you really don’t want to talk about, and you’re very, very private with how you handle a day that has [00:31:00] taken everything you’ve got out of you and you’ve seen just way too much tragedy and And you’ve listened to the stories and you know what’s ahead of that woman. So how do you take care of Laura?
Laura: Well, the first thing that I do when I leave here is once I get in the car, I do turn my radio up loud and roll the windows down and just try to have a me moment. Uh, most of the time, just singing along to the music, kind of, winds me down. And when I get home to my family, it’s like, I’m not cooking today. We’re going out or you’re cooking, or most of the time my daughter, she likes to cook. So I got very lucky with that. So I wind down by being with my family, just friends, family, you know, just being grateful for everything that I have.
And, um, We hear a lot of sad stories and a lot of times they stick with us and it’s it’s very sad What us as humans can do good and bad. [00:32:00] So it’s always nice to try to keep it level and try to help those in need and That’s what we’re here for.
Dorothy: Mm hmm. I know we’ve taken women who were in shelters And didn’t know where they were going to go and y’all found help for that one.
I remember that one was so well, two kids and didn’t know what was going to happen to her. And y’all found resources for her. The homeless lady that we had to find a phone so that she could even make her appointments. Yes, but, but there are so many different needs, so many different stories. And I guess The Rose family, we’ve learned that.
That we better appreciate each other, and love each other, and be there for each other. So, anyone that’s facing breast cancer, or any kind of cancer, there are so many things that are going to go through your mind. So many fears, and that’s all normal as it should be, [00:33:00] but if you come to The Rose and talk to these two ladies, you’re going to have a friend to get you through the treatment.
Thank y’all so much for being with us today, for sharing your stories and, um, for making us cry. That’s it for today.
Laura: Thank you.
Sally: Thank you.
Post-Credits: Thank you for joining us today on Let’s Talk About Your Breasts. This podcast is produced by Freddie Cruz Creative Works and brought to you by The Rose. Visit TheRose.org to learn more about our organization.
Subscribe to our podcast, share episodes with friends, and join the conversation on social media using #Let’sTalkAboutYourBreasts. We welcome your feedback and suggestions. Consider supporting The Rose. Your gift can make the difference to a person in need. And remember, self care is not selfish.
It’s essential.