Dorothy: [00:00:00] Dr. Raz and I usually agree on things, but not in this episode. We’re discussing breast cancer in young women. These are the women who are under 40 years old, women who have been told they are too young to have a routine mammogram, the same women who are eventually diagnosed with breast cancer, and many times that is at a later stage.
So, is the incidence of breast cancer in younger women increasing or not? Our lead radiologist, Dr. Raz, agrees that there may be an increase, and it might be a trend. I insist it is, and it’s an alarming trend. While I want women to be able to have a screening mammogram at any age, Dr. Raz doubts that changing the recommended age for starting mammograms will make a difference. However, he does have another solution, and you’ll hear it today on Let’s Talk About Your Breasts.
When you subscribe to our show, you help us grow. Someone you know may [00:01:00] need to hear this story. So please share with your family and friends and consider supporting our mission at therose.org.
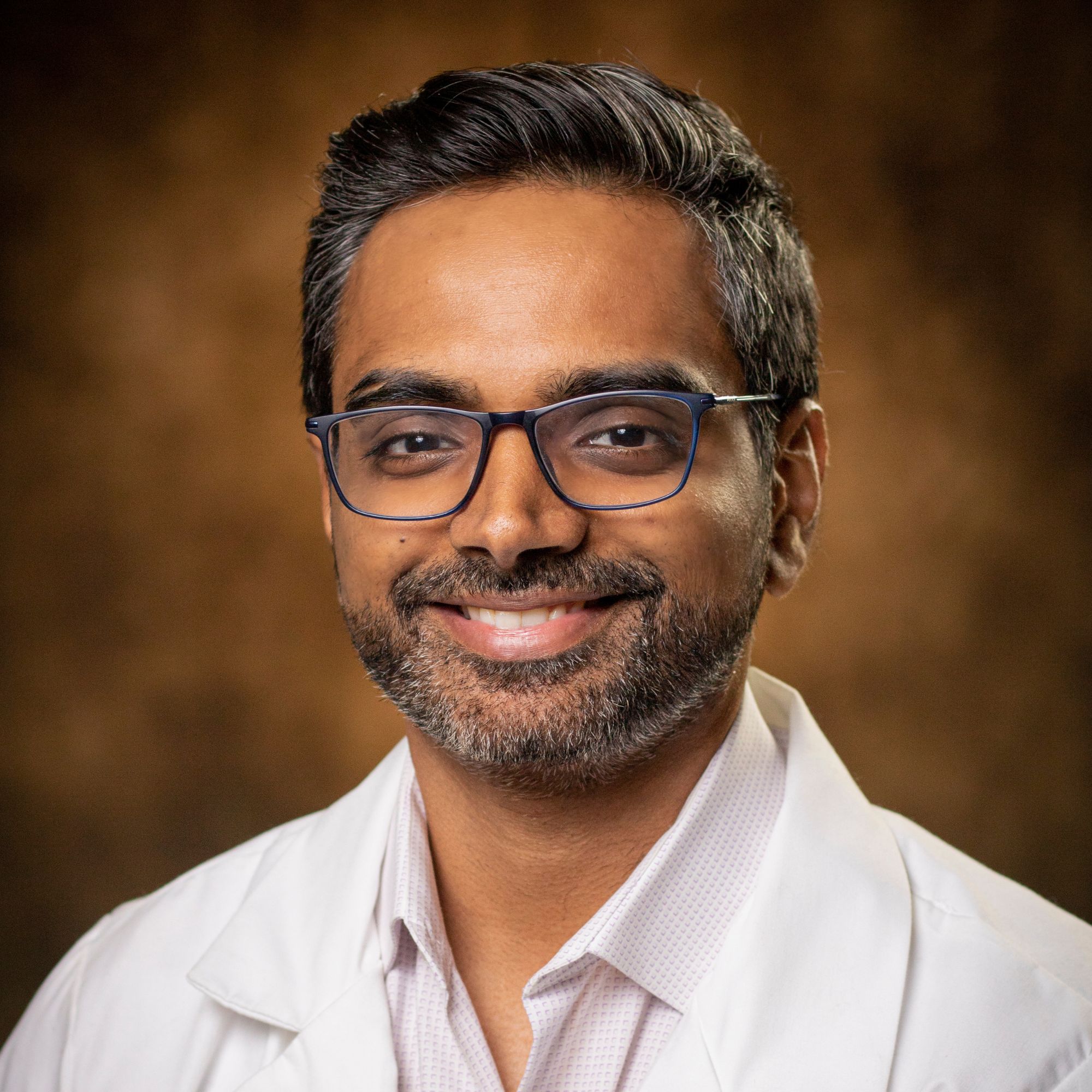
Let’s Talk About Your Breast, a different kind of podcast presented to you by The Rose, the Breast Center of Excellence and a Texas treasure. You’re going to hear frank discussions about tough topics, and you’re going to learn why knowing about your breast could save your life.
Dr. Raz and I are talking about has cancer increased in younger women? I say we’re seeing more here at The Rose.
Dr. Raz: Yeah, we are seeing more.
Dorothy: Okay, okay, but he says that that’s not incidents, that there’s a whole other formula to ever coming up with this stuff?
Dr. Raz: Yeah.
Dorothy: Explain that part to us.
Dr. Raz: Well, so, you know, incidents generally refers to the fact that how many cancers we’re catching.
Dorothy: Okay.
Dr. Raz: And you know, obviously incidents has increased. There’s a base rate of [00:02:00] increase of incidents every year for breast cancer, whether you’re over 40 or under 40.
Dorothy: Okay.
Dr. Raz: So it’s a dual-edged thing where the increase in incidence is because our screening methodologies have been better. Then there is new, um, you do great outreach here at The Rose and all these other centers throughout the U. S., so more women are screening, hence we’re catching more cancer. The question remains, has there been an increased basal rate of cancer itself, even if we don’t screen? That’s a difficult question to answer. However, we do know that the incidence of cancer in younger women under 40 has been increasing around 1%. So again, the question is whether are they, are they more conscious about it?
Dorothy: But we’re not screening. We’re not screening these women.
Dr. Raz: Right, we’re not screening. But they may know about it and then they do self breast exam when they come in and then we find masses and those turn out to be cancer, if that makes sense.
Dorothy: Okay, so, we’re never going to get the recommendations changed based on scientific evidence is what you’re saying.
Dr. Raz: Correct. Like the age, because it’s a, it’s a risk reward [00:03:00] thing. So if you reduce the age, let’s say from 40 to 35, right? For screening.
Dorothy: Okay, okay.
Dr. Raz: What will end up happening is we’ll have way more false positives, meaning we’ll biopsy a whole bunch and then we’ll catch cancer. So it’s, remember, screening, um, is a national program, so you have to get through a lot of red tape. This is not my recommendation.
Dorothy: I know.
Dr. Raz: I would, I would rather catch, so you’ll catch more cancers.
Dorothy: Yes.
Dr. Raz: Now for that matter, you know, we screen once a year, right? There have been studies that show if you screen twice a year, you catch more cancer. Exactly. Yes. So there are studies I could, I mean, I don’t know the name of them, but I know of them. They’re good studies from reputable academic centers that yeah, if you do screening twice a year, you catch more cancers. But again, it’s a risk reward thing. How much burden on healthcare would there be if we do that?
Dorothy: Until it’s your life.
Dr. Raz: You are absolutely correct. Until it’s your life. Yes.
Dorothy: Okay. So if you had your way, what do you think would be the better way to screen?
Dr. Raz: So the— you know, the [00:04:00] general screening guidelines for, that we start at 40, you know, uh, these studies were made way back then, and, you know, it’s, the subgroups weren’t as defined, you know, United States.
Dorothy: So explain what you said about, these studies were all done on primarily white women?
Dr. Raz: That’s correct.
Dorothy: Who were insured.
Dr. Raz: Yes, compliant to screening. Yes, compliant to screening. So all of this really makes it difficult and there, there’s no great way to come up with an age, unfortunately, but this is the best we can come up with.
Ideally, what you do is, and this is how you catch cancer under 40. And again, remember, we talked about it, that the incidence has increased. Now, whether that’s because women are more conscious or there’s just this something wrong and we’re all getting more cancers, difficult to know.
Dorothy: Okay.
Dr. Raz: Um, But let’s just assume there’s something happening where a lot of younger women are getting breast cancer. You know, the risk factors are many. Many could be, you know, um, early, uh, [00:05:00] menarche or, you know, you didn’t have kids or obviously, you know, family history or genetics, but these other things that I’m saying, you know, breastfeeding, not breastfeeding, you know, null parity, meaning you didn’t have kids.
All of these are minor risk factors for developing breast cancer. What I’m trying to get to is, if there is increased risk of due to various factors that we don’t know yet, how do we catch it? Well, The thing is there are subgroups within women. So whether, you know, you’re, you know, your socioeconomic status, that’s actually a subgroup.
Then, then race, right? So we know for a fact that women that are under 40 who are black women tend to get larger cancers if they were to get it, more aggressive cancers, and triple negative breast cancer, which has poorer prognosis. So that’s not as well studied. So this is the thing, like at the primary care level, when a physician speaks with a woman, there has to be an easier tool.
Like here at The Rose, what do we have? You know, we have Amanda, we have a [00:06:00] nurse practitioner, and they go through and she has excellent tools. She has tire cruising model and gill model. These are just models that risk stratify a woman, whether you’re high risk or not. At a primary care, do these primary cares have that sort of tool? I don’t think so. It’s not very easy. I don’t expect primary care physicians to know all these nuances of breast imaging and Breast Risk Stratification, but if on a national basis, let’s say we can come up with more nuanced under 40 risk stratification model of some sort, which then filters these women that hey, you are actually higher risk than an average American woman risk which average American woman risk is 1 in 8, then that would really help catch cancers early.
Dorothy: Okay, so what you’re saying is if we had true high risk screening.
Dr. Raz: Correct.
Dorothy: That could be applied population wide.
Dr. Raz: Correct.
Dorothy: Then we would be able to say this subset of women needs to start at 3. [00:07:00]
Dr. Raz: Earlier, yes, earlier. Earlier screening or different methodology. I mean, that’s all science. We can all study that. Or whether we start with ultrasound, mammogram, or MRI. Ideally, it would be MRI for higher risk women. Yes, and in an easier way to risk stratify women at an early age, so then we can say, hey, you can start early, would actually yield benefit.
Dorothy: So what would speed up that process?
Dr. Raz: Well, loaded question.
Dorothy: I know. So again, look how long we’ve been dealing with age 40, then it went to age 50, now it’s back to age 40.
Dr. Raz: And it was bi annual, then it’s, you know, I mean not bi annual, every other year.
Dorothy: Every other year.
Dr. Raz: Then, and one year, uh, every year. So, really it’s um, you know, USPSTF and the, you know, the Surgeon General, everything, it’s, you know, there has to be consensus on that level, honestly. Well, because they make the [00:08:00] standard rules. They make all these rules that, you know, when should we screen and every insurance provider follows it.
Dorothy: I mean, I know that, but what I’m saying is, Why? Why can’t a woman just say, I want to have a mammogram?
Dr. Raz: Yeah, they can. I mean, we see plenty of women that are at 30 that come in, but again, it’s, it’s a matter of education, right? And this also feeds into incidents, as you said, a lot of women are doing that now.
Dorothy: Only because they have awareness.
Dr. Raz: Correct.
Dorothy: Are they become aware that they actually have a problem going on?
Dr. Raz: Yes.
Dorothy: Are, what’s the mother’s, family history or?
Dr. Raz: So family history, and again, a lot of this is just awareness in general. People, you know, women listening to your podcast, see? So that’s, all of this helps.
Dorothy: Yes. But at the end of the day, she’s still going to need a physician order.
Dr. Raz: That’s correct.
Dorothy: Whether she’s insured or uninsured, she’s still going to need someone with a medical degree to [00:09:00] say you need a mammogram. She can’t just decide that.
Dr. Raz: No, no. And that’s where the sole risk stratification and a physician saying, Hey, you’re a higher risk, go do mammogram comes in. How do we implement that? Difficult to do. Again, it comes from higher levels. All these societies then have to come up with their guidelines and send it to their physician. And that’s how we do things, right?
So like Society of Breast Imaging, these are all of us. ACOG is American College of Oncology and Gynecology. So. There is a society for family practice physicians and also internal medicine. And all that gets filtered really through USPSTF, Surgeon General and stuff. So, so we’re, what I’m trying to get to isn’t, I’m not trying to be negative.
I’m just trying to come up with practical solutions. And that’s, you know, from our local level in the community level, what you’re doing in podcasts. And we talk with, I talk with primary care physicians all the time and I’m educating them. That’s also part of the reason that we see, you [00:10:00] know, decent amount of younger women under 40, with complaints, obviously. But I mean, yes, if every breast imagery went out there and started doing this, that would be helpful on a community level, on a local level.
Dorothy: But it really takes policy.
Dr. Raz: Yes, it does.
Dorothy: No matter what.
Dr. Raz: Because nationally, that’s how we do it, right? Start at 40. Who decides that? ACR does, American College of Radiology, right? USPSTF does.
Dorothy: And the insurance control it.
Dr. Raz: Correct.
Dorothy: And?
Dr. Raz: And they look at the, the national policy. So.
Dorothy: All right. So what other great news do you have for us today as we start out 2025?
Dr. Raz: Well, the, well, the great news from, from The Rose perspective, I could tell you is, you know, we’re doing a lot more MRI. So, MRI is firing on all cylinders right now and I’m reading at least two, three every week.
And, you know, we’re getting to good MRIs, good problem solving, caught couple of cancer [00:11:00] in younger women that way for high risk women. And, um, you know, the, the, the other great news would be, um, you know, there’ve been recent papers that are coming up with, contrast enhanced tomography, right? So it’s something that we’re also working on at Rose a few months away, but that is showing excellent promise.
So something that we look at is called cancer detection rate and cancer detection rate on this, this new modality is up to par with almost MRI. So lots of centers have started aggressively doing it. Just speaking with my colleague at Baylor, they just started a month ago.
Dorothy: Ah.
Dr. Raz: So, which is Smith Clinic, so Baylor. And they’re getting excellent results. They’re starting, you know, keeping documentation of all of this. So, So that would really help and you were just tying it back to younger women and if you’re high risk women, you know, this would really be an excellent study because remember the problem with MRI is [00:12:00] compliance.
Dorothy: Mm hmm.
Dr. Raz: And this would completely solve it.
Dorothy: So what is contrast enhanced mammography?
Dr. Raz: Right. So Contrast enhanced mammography, we all know what mammography is. So specifically, it’s not even mammography, it’s tomography. So 3D mammogram. Well, with contrast enhanced mammography, we inject contrast and iodine based contrast.
Dorothy: Very much like—
Dr. Raz: When you go get a CT.
Dorothy: Right.
Dr. Raz: You know, CT abdomen, pelvis, if you’re getting CT brain.
Dorothy: Yeah, yeah.
Dr. Raz: Or if you’re even getting MRI, they inject contrast. And the goal of contrast is, well, it’s easy, layman terms would be, if there’s cancer, it would enhance. It will turn white. Versus tissue would not turn white, right? Color wise, if you’re speaking, it will take up color. This is the color. Iodine or contrast is the color. So then it’s very easy to pick up subtle cancers. A lot of times cancer height, especially again in younger women, um, uh, dense breast, you know, dense breast, you can hide many things, which is why we were saying, you know, this [00:13:00] new stipulation that we have to talk about breast density in all of our letters. is because breast density, unfortunately, is an independent risk factor of breast cancer.
Dorothy: Okay, but remember the USPSTF.
Dr. Raz: Right. So.
Dorothy: Tell me.
Dr. Raz: Yeah, so that.
Dorothy: They didn’t approve it as a supplemental study as needing that.
Dr. Raz: Not yet, but this is how a change happens, Dorothy. It starts like this. I’m being honest. It starts like this. And a lot of these women, You know, few will get this letter and then they’ll go do ultrasound and we’ll catch something. And then this is how it works. I mean, unfortunately it’s a slow process. This is what medicine is in general. It’s a slow tanker. This is not a tech company. Like overnight we’re making new tools and then there’s a CEO.
It’s just a slow thing. Takes a while, but these are all encouraging things. Sending that letter. That’s actually an exciting development in and of itself.
Dorothy: It is.
Dr. Raz: Because we’re doing more [00:14:00] ultrasound. We already proved that, hey, If dense women, dense breast, breasted women come in and I do mammogram and ultrasound, if I just do mammogram, I catch cancer in three out of a thousand. If I had ultrasound, I catch five out of a thousand. I’m catching two extra cancer. And again, what did you just say? Unless it’s your life.
Dorothy: Unless it’s your life.
Dr. Raz: Yeah. So then out of those two women, they for sure will know that, Hey, without ultrasound, it wouldn’t have been caught.
Dorothy: Right.
Dr. Raz: Again, kind of getting off topic, but that contrast enhanced mammography, It just adds to this detection rate.
Dorothy: It’s in between there almost.
Dr. Raz: That’s correct.
Dorothy: It’s another one. Yeah.
Dr. Raz: Correct. It’s even, it’s very sensitive. It’s very sensitive and cancer detection rate is as good as MRI. Remember, MRI is better than ultrasound. It’s almost as good as MRI. Well, then this will become the gold standard. Eventually. Again, take some time. Studies need to come. Again, you’re right. USPSTF. They’ll, they’ll — it gets drilled into their brain that it is beneficial. It takes them a few years.
Dorothy: It may take them a lot more years [00:15:00] before all of this happens.
Dr. Raz: I’ll, I’ll send them a link to your podcast.
Dorothy: Cause you know, I feel very strongly that, that we just need a lot better ways to take care of women.
Dr. Raz: Yeah, I agree with you.
Dorothy: I know we, I know it’s because more women come in with a problem, I know that. But my gosh, the difference in our population, the uninsured and the insured. You know, we diagnose the same number every year.
Dr. Raz: Yes.
Dorothy: That’s just amazing to me. And often, you do see more pathology here than you have before, right?
Dr. Raz: That’s correct, yeah.
Dorothy: And explain what that means.
Dr. Raz: So. So, you know, the patient population that comes through a screening program, whether it be at The Rose or any other academic, tends to be a little different because it’s, you know, related to socioeconomic status, your age.
So, the pathology that comes in here, we take care of so many uninsured women [00:16:00] here, Tends to be, you know, cancer that could be a little bit later stage, a little bit aggressive and sometimes just exotic. Just the other day, there was like a mixed soy cancer that I had. And yeah, so that’s, it tends to be non geographic, right?
A lot of, you know, patients do coming from South America here. So the cancer morphology is a bit different. So we tend to see a little bit of different Pathology and let’s say a patient that goes to Methodist if you will. Um, so, yeah. That’s, that’s what it really means.
Dorothy: Yeah, and because of that it’s more important for us to get him on antitreatment, cause some of these are very aggressive.
Dr. Raz: No, some are very aggressive, especially, you know, and I’m completely with you, like it’s, it’s an open question, especially for women under 40. What to do.
Dorothy: I knew you were with me on that.
Dr. Raz: Yes. I’m just.
Dorothy: I, I just know we’ve gotta do something different.
Dr. Raz: Correct.
Dorothy: For that.
Dr. Raz: Um, and they, and this is a fact, and [00:17:00] even USPSCF can deny this, that they just get more aggressive cancers. Which will make sense that, well, because breast cancer is supposed to be an older woman’s disease, so if you get it at a younger age, something’s wrong. So it tends to be germline mutation, meaning some genetic mutation or how you’re born. Um, and then these cancers just tend to be very aggressive. So you got to move in fast.
Dorothy: And I know this is another point that we don’t always agree on. But we have seen so many pregnant.
Dr. Raz: Yes.
Dorothy: Are just had babies or babies that are five years old or younger.
Dr. Raz: Yes.
Dorothy: Peripartum. Isn’t it time for us to do a little more awareness on that?
Dr. Raz: So peripartum cancer is often missed, unfortunately. And it’s missed because the breast that, you know, again, there’s two organs that are the most sensitive to estrogen and changes a lot in a woman. And this is interesting. A lot of women, you know, sometimes I tell patients this too. If I were to do biopsy on a [00:18:00] breast every single day, let’s say I pick a woman to start biopsying the tissue day one, two, three, four, all 28 days. Okay. And looking at a microscope, the breast will look different every day. It’s kind of like a uterus. So what does uterus go through? You know, it’s preparing for pregnancy every month in a woman, right? And you don’t get pregnant. You get the period and then cycle repeats. So the uterine lining changes every day.
Because it’s under the influence of estrogen and progesterone. Well, then same thing happens to breasts. These are the two most sensitive organs to cycles, right? That a woman goes through. Where am I getting to? Well, at pregnancy, an estrogen is like 10x than a normal woman would. Why? Because it’s maintaining the pregnancy. Right?
Dorothy: Okay.
Dr. Raz: Now, so the breast looks very different, it’s very engorged, it’s preparing for lactation, all of that. So you feel lots of lumps and bumps. Well then how would you know which lump is good or which lump is not? So a lot of [00:19:00] times what ends up happening in primary care just does their exam and then they’re like, well, it looks like just like a pregnant breast or, you know, lactating breast.
And they kind of let it go. And fortunately, that’s exactly where cancer, and remember, cancer loves estrogen. Majority, we are positive cancers. It’s like a fat kid with cake, you know, nom, nom, nom. And it increases in size explosively. Remember, in pregnancy, you have 10x the estrogen. So then you’re explosively growing mass, and then it gets missed.
The woman’s already busy. This is where it comes in. You know, we need to take better care of women. Why? Because she’s already working a job, pregnant, taking care of, she’s like, eh, it’s probably nothing. And then my doctor said it was nothing, the primary care, and then now, well lo and behold, you know, this, like an aggressive grade 3, you know, stage 2, 3 cancer, and it was completely missed because of the situation I explained, and this happens all the time.
Dorothy: So it’s important for a woman to say, no, I think this is different.
Dr. Raz: That is correct, and that’s the majority of the [00:20:00] peripartum cancers I’ve caught. Where a woman comes like, no, this feels different, you know, unfortunately. And it’s almost always, it’s very, it’s very sad. It makes me sad because a lot of these women are in their thirties.
It’s having their second kid or just had one kid. So yeah, the, you know, that’s, we can definitely talk a lot about this. on the next podcast and because the cancer and the way peripartum breasts should be imaged and it’s, it’s, it’s a whole different topic.
Dorothy: Oh, good. A very sensitive topic. We agree on something here that we can talk about. All right, you’re on. I’ll bring you back and we’ll talk just about what happens when a woman’s pregnant.
Dr. Raz: Yes.
Dorothy: Or even the years afterwards.
Dr. Raz: That’s correct. Yeah. Peripartum, plus or minus around childbirth. The breast is different. The pathology is different. The physiology is different than a regular woman. Yeah.
Dorothy: Oh, good. And you can get us maybe some images so we can see it.
Dr. Raz: Yes, for sure. I have lots.
Dorothy: Well, then you’re on. We’ll have you back, Dr. Raz. Thank you so much for today.
Dr. Raz: Pleasure is all mine. Thank you for [00:21:00] having me.
Post-Credits: Thank you for joining us today on Let’s Talk About Your Breasts. This podcast is produced by Speke Podcasting and brought to you by The Rose. Visit therose.org to learn more about our organization. Subscribe to our podcast, share episodes with friends, and join the conversation on social media using #LetsTalkAboutYourBreasts. We welcome your feedback and suggestions. Consider supporting The Rose. Your gift can make the difference to a person in need. And remember, self care is not selfish. It’s essential.